Telemedicine, a key component of the broader telehealth movement, has transformed how healthcare services are delivered, especially in the context of modern technology and growing patient expectations. By using telecommunications technology, telemedicine allows for remote consultations, diagnosis, treatment, and management of healthcare needs. From improving access to care, enhancing convenience, and reducing costs, to addressing significant challenges such as healthcare inequalities and a shortage of medical professionals in certain regions, telemedicine has made a significant impact on the healthcare industry.
Telemedicine’s evolution over the past few decades, especially with the advancement of internet access, mobile technology, and artificial intelligence (AI), makes it a cornerstone of modern healthcare systems. This article delves into the role of telemedicine in today’s healthcare environment, focusing on its benefits, challenges, and future prospects.
The Growth of Telemedicine
Telemedicine has been a part of the healthcare landscape for years but has seen rapid growth in the last decade due to a variety of factors:

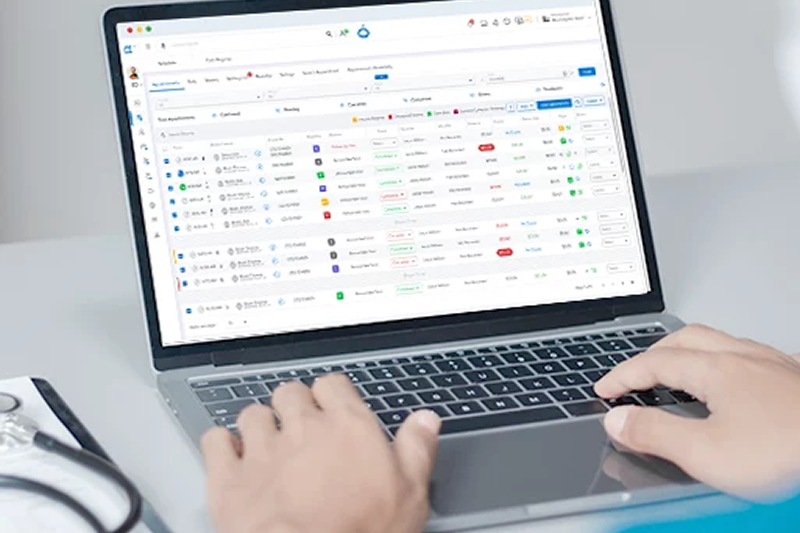
- Advances in Technology: The development of high-speed internet, improved video conferencing tools, wearables, and mobile applications have played a critical role in making telemedicine services efficient and accessible. With more reliable digital platforms for patient-doctor communication, telemedicine has become viable on a global scale.
- Increased Demand for Convenience: As patient expectations evolve, people seek more convenience and flexibility in how they access healthcare. Telemedicine allows consultations to happen without patients needing to leave their homes, thus avoiding time-consuming travel, waiting in lines, or taking time off work.
- COVID-19 Pandemic: The global health crisis highlighted the need for safe, accessible healthcare options without in-person visits. During this time, telemedicine saw unprecedented growth, becoming not only a necessary service but also a preferred method of accessing medical care. Despite its initial growth spurts during this period, many patients and healthcare providers discovered long-term advantages, leading to its sustained use post-pandemic.
Key Benefits of Telemedicine
Telemedicine offers various advantages to both patients and healthcare providers.
1. Improved Access to Healthcare
One of the primary advantages of telemedicine is its ability to bridge geographic and logistical barriers to healthcare. Telemedicine enables patients who live in remote or underserved areas to access medical services from specialized doctors and specialists that would otherwise be unavailable.
For rural populations, where there may be fewer healthcare facilities, telemedicine brings expert opinions to those who need them most. Rural health issues like a shortage of healthcare workers and specialists can be mitigated through virtual healthcare visits, ensuring continuity of care and support.
2. Enhanced Convenience and Cost Savings
Patients benefit significantly from the convenience of telemedicine. With busy lifestyles and work commitments, individuals may find it challenging to attend in-person appointments. Telemedicine eliminates these obstacles by providing flexibility in scheduling and locations.
The Benefits of Lifelong Learning: Why Continuous Education Matters
Additionally, both patients and healthcare providers can save money with telemedicine. Patients save on transportation costs, daycare fees, and time off work, while healthcare providers reduce overhead by cutting down on office maintenance, staff, and equipment needs. Moreover, health insurers have increasingly supported telemedicine services, making virtual care a more financially viable option for many individuals.
3. Enhanced Continuity of Care and Chronic Disease Management
Telemedicine’s real-time monitoring features allow healthcare providers to check on patients more frequently and manage their chronic conditions better. For individuals dealing with long-term illnesses such as diabetes, hypertension, or heart disease, telemedicine is a vital tool for monitoring symptoms, adjusting medications, and providing lifestyle recommendations without requiring frequent hospital visits.
Telemedicine platforms, often supported by mobile applications and devices, allow patients to track their conditions. Whether it’s monitoring blood sugar levels, heart rates, or other crucial health data, this integration into daily life leads to more personalized treatment plans. Real-time consultations give healthcare providers the opportunity to intervene sooner when a condition is exacerbated.
4. Faster Diagnosis and Reduced Waiting Times
Traditional healthcare systems often require patients to endure long wait times for consultations and diagnoses. Telemedicine addresses this issue by allowing virtual consultations that can take place from anywhere, cutting down wait times for appointments or treatments. This increased speed ensures patients receive the attention they need promptly, reducing the time between diagnosis and treatment, which is crucial in some medical cases.

5. Reduction in the Risk of Healthcare-Associated Infections
Telemedicine greatly reduces the likelihood of exposure to infectious diseases by allowing patients to consult with doctors remotely. In situations like the COVID-19 pandemic, virtual healthcare services are essential in keeping patients out of clinical environments where infections might spread. Telemedicine ensures continuity of care, particularly for non-urgent conditions, minimizing physical contact.
6. Supporting Mental Health Care
Telemedicine also plays a vital role in expanding access to mental health services, which are often underrepresented in traditional healthcare systems. Patients dealing with mental health issues, especially in areas with limited mental health resources, find telemedicine consultations to be an easy and accessible way to seek therapy and counseling without facing stigma or geographical limitations.
Challenges and Limitations
Despite its significant benefits, there are also several challenges and limitations to telemedicine that must be addressed for its continued growth and success.
1. Technological Barriers
For telemedicine to work effectively, it depends on reliable technology. Many areas still struggle with inconsistent internet access, hindering patients in rural or low-income regions from accessing quality remote healthcare. In some cases, patients may lack access to the required devices, such as smartphones or computers, further limiting their ability to use telemedicine platforms.
Additionally, some telemedicine technologies require users to have technical knowledge to set up devices or troubleshoot problems. For elderly patients or those who are not tech-savvy, this poses a substantial barrier to adoption.
Connecting the World Through Education: The Role of Technology
2. Legal and Regulatory Issues
Telemedicine is also hindered by varying state, regional, and national regulations. Health professionals providing care remotely must comply with regulations that can differ depending on the patient’s location. This includes licensing, reimbursement models, privacy protection, and other regulations tied to remote services.
In particular, there is a complex issue of reimbursement for telemedicine services. While many insurance companies and government programs, such as Medicare, have expanded coverage for telemedicine services, there are still discrepancies that need addressing in terms of reimbursement rates, cross-state care, and policies that support long-term sustainability.
3. Security and Privacy Concerns
Security remains a central concern, as sensitive health data is transmitted via online platforms. The use of telemedicine can potentially open the door to cyberattacks and data breaches. To overcome this, healthcare providers and developers of telemedicine technology must implement strict cybersecurity measures and adhere to regulations like the Health Insurance Portability and Accountability Act (HIPAA) to protect patient privacy.
Patients might feel uneasy about the safety of their medical information being shared online, leading to reluctance in embracing telemedicine.
4. Limited Physical Examination
While telemedicine has made substantial progress in the virtual healthcare space, it has limitations, particularly for conditions requiring a physical examination. Some diagnoses, such as detecting physical abnormalities or injuries, can only be performed in person. In these cases, telemedicine serves as an initial point of contact and can guide patients toward in-person care when necessary.
5. Equity Concerns
Despite the increased availability of telemedicine, there remains an issue of equity. Telemedicine heavily relies on technology infrastructure, and individuals without access to the right tools or internet connection are often excluded. Additionally, certain populations, such as those with disabilities or non-English speakers, may face additional challenges with using telemedicine effectively without the proper accommodations in place.
The Future of Telemedicine
The future of telemedicine looks promising, with several advancements on the horizon that can enhance patient care, bridge the equity gap, and improve efficiency in healthcare delivery.
1. Artificial Intelligence (AI) and Machine Learning Integration
The integration of AI and machine learning into telemedicine platforms will allow for more accurate diagnosis, predictive analytics, and personalized treatment plans. AI can help process data quickly, alert healthcare professionals to patient risks, and offer suggestions for medical interventions. Additionally, AI-powered virtual assistants can improve the patient experience, enhancing triage efficiency and patient support throughout the consultation process.
2. Wearables and Remote Patient Monitoring
The integration of wearable devices, such as smartwatches that monitor vital signs or glucose levels, provides a continuous stream of real-time data that can be analyzed by doctors in virtual consultations. In the coming years, remote patient monitoring systems will become more advanced, enabling healthcare providers to manage chronic conditions, track recovery, and prevent complications from the comfort of their own homes.
3. Global Expansion of Telemedicine
Telemedicine will continue to expand across borders, especially in underserved regions. Initiatives like the World Health Organization’s (WHO) efforts to provide essential medical services globally through telemedicine systems may increase accessibility in remote areas. Overcoming regulatory barriers will make it easier for patients to access global medical expertise, regardless of their location.
4. Expanding Insurance Coverage
As telemedicine proves its value, it’s likely that more insurance companies and national health systems will include it as a viable and reimbursed option. Expanding telemedicine’s inclusion in healthcare plans will ensure more widespread access to care, particularly for non-urgent consultations and follow-up visits.
The Impact of International Partnerships in E-Learning Development
Telemedicine is playing a crucial role in modern healthcare systems. By offering more efficient, cost-effective, and convenient access to care, it’s helping reshape the way healthcare is provided. Although challenges remain, the growing integration of advanced technologies, greater access to digital platforms, and ongoing regulatory adaptations suggest that telemedicine will continue to be an essential part of healthcare delivery in the future. With careful planning and development, telemedicine will reach its full potential in making healthcare more accessible and equitable for everyone, irrespective of geographical location or economic status.

